Definition
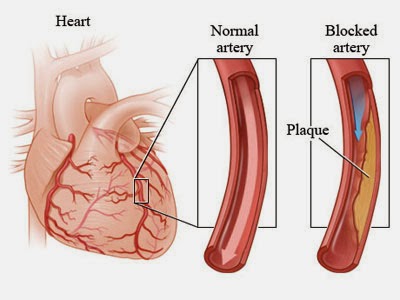
Coronary artery disease develops when your coronary arteries — the major blood vessels that supply your heart with blood, oxygen and nutrients — become damaged or diseased. Cholesterol-containing deposits (plaque) in your arteries and inflammation are usually to blame for coronary artery disease.
When plaques build up, they narrow your coronary arteries, decreasing blood flow to your heart. Eventually, the decreased blood flow may cause chest pain (angina), shortness of breath, or other coronary artery disease signs and symptoms. A complete blockage can cause a heart attack.
Because coronary artery disease often develops over decades, it can go unnoticed until you have a heart attack. But there's plenty you can do to prevent and treat coronary artery disease. Start by committing to a healthy lifestyle.
Symptoms
If your coronary arteries narrow, they can't supply enough oxygen-rich blood to your heart — especially when it's beating hard, such as during exercise. At first, the decreased blood flow may not cause any coronary artery disease symptoms. As the plaques continue to build up in your coronary arteries, however, you may develop coronary artery disease signs and symptoms, including:
- Chest pain (angina). You may feel pressure or tightness in your chest, as if someone were standing on your chest. The pain, referred to as angina, is usually triggered by physical or emotional stress. It typically goes away within minutes after stopping the stressful activity. In some people, especially women, this pain may be fleeting or sharp and felt in the abdomen, back or arm.
- Shortness of breath. If your heart can't pump enough blood to meet your body's needs, you may develop shortness of breath or extreme fatigue with exertion.
- Heart attack. A completely blocked coronary artery may cause a heart attack. The classic signs and symptoms of a heart attack include crushing pressure in your chest and pain in your shoulder or arm, sometimes with shortness of breath and sweating. Women are somewhat more likely than men are to experience less typical signs and symptoms of a heart attack, such as nausea and back or jaw pain. Sometimes a heart attack occurs without any apparent signs or symptoms.
When to see a doctor
If you suspect you're having a heart attack, immediately call 911 or your local emergency number. If you don't have access to emergency medical services, have someone drive you to the nearest hospital. Drive yourself only as a last resort.
If you have risk factors for coronary artery disease — such as high blood pressure, high cholesterol, tobacco use, diabetes or obesity — talk to your doctor. He or she may want to test you for the condition, especially if you have signs or symptoms of narrowed arteries. Even if you don't have evidence of coronary artery disease, your doctor may recommend aggressive treatment of your risk factors. Early diagnosis and treatment may stop progression of coronary artery disease and help prevent a heart attack.
Causes
Multimedia
Coronary artery disease is thought to begin with damage or injury to the inner layer of a coronary artery, sometimes as early as childhood. The damage may be caused by various factors, including:
- Smoking
- High blood pressure
- High cholesterol
- Diabetes or insulin resistance
- Radiation therapy to the chest, as used for certain types of cancer
- Sedentary lifestyle
Once the inner wall of an artery is damaged, fatty deposits (plaques) made of cholesterol and other cellular waste products tend to accumulate at the site of injury in a process called atherosclerosis. If the surface of these plaques breaks or ruptures, blood cells called platelets will clump at the site to try to repair the artery. This clump can block the artery, leading to a heart attack.
Risk factors
By Mayo Clinic Staff
Risk factors for coronary artery disease include:
Age. Simply getting older increases your risk of damaged and narrowed arteries.
Sex. Men are generally at greater risk of coronary artery disease. However, the risk for women increases after menopause.
Family history. A family history of heart disease is associated with a higher risk of coronary artery disease, especially if a close relative developed heart disease at an early age. Your risk is highest if your father or a brother was diagnosed with heart disease before age 55 or your mother or a sister developed it before age 65.
Smoking. Nicotine constricts your blood vessels, and carbon monoxide can damage their inner lining, making them more susceptible to atherosclerosis. The incidence of heart attack in women who smoke at least 20 cigarettes a day is six times that of women who've never smoked. For men who smoke, the incidence is triple that of nonsmokers.
High blood pressure. Uncontrolled high blood pressure can result in hardening and thickening of your arteries, narrowing the channel through which blood can flow.
High blood cholesterol levels. High levels of cholesterol in your blood can increase the risk of formation of plaques and atherosclerosis. High cholesterol can be caused by a high level of low-density lipoprotein (LDL), known as the "bad" cholesterol. A low level of high-density lipoprotein (HDL), known as the "good" cholesterol, also can promote atherosclerosis.
Diabetes. Diabetes is associated with an increased risk of coronary artery disease. Both conditions share similar risk factors, such as obesity and high blood pressure.
Obesity. Excess weight typically worsens other risk factors.
Physical inactivity. Lack of exercise also is associated with coronary artery disease and some of its risk factors, as well.
High stress. Unrelieved stress in your life may damage your arteries as well as worsen other risk factors for coronary artery disease.
Risk factors often occur in clusters and may build on one another, such as obesity leading to diabetes and high blood pressure. When grouped together, certain risk factors put you at an even greater risk of coronary artery disease. For example, metabolic syndrome — a cluster of conditions that includes elevated blood pressure, high triglycerides, elevated insulin levels and excess body fat around the waist — increases the risk of coronary artery disease.
Sometimes coronary artery disease develops without any classic risk factors. Researchers are studying other possible factors, including:
Sleep apnea. This disorder causes you to repeatedly stop and start breathing while you're sleeping. Sudden drops in blood oxygen levels that occur during sleep apnea increase blood pressure and strain the cardiovascular system, possibly leading to coronary artery disease.
C-reactive protein. C-reactive protein (CRP) is a normal protein that appears in higher amounts when there's swelling somewhere in your body. High CRP levels may be a risk factor for heart disease. It's thought that as coronary arteries narrow, you'll have more CRP in your blood.
High triglycerides. This is a type of fat (lipid) in your blood. High levels may raise the risk of coronary artery disease, especially for women.
Homocysteine. Homocysteine is an amino acid your body uses to make protein and to build and maintain tissue. But high levels of homocysteine may increase your risk of coronary artery disease.
Lipoprotein (a). This substance forms when a low-density lipoprotein (LDL) particle attaches to a specific protein. Lipoprotein (a) may disrupt your body's ability to dissolve blood clots. High levels of lipoprotein (a) may be associated with an increased risk of cardiovascular disease, including coronary artery disease and heart attack.
Complications
Coronary artery disease can lead to:
- Chest pain (angina). When your coronary arteries narrow, your heart may not receive enough blood when demand is greatest — particularly during physical activity. This can cause chest pain (angina) or shortness of breath.
- Heart attack. If a cholesterol plaque ruptures and a blood clot forms, complete blockage of your heart artery may trigger a heart attack. The lack of blood flow to your heart may damage your heart muscle. The amount of damage depends in part on how quickly you receive treatment.
- Heart failure. If some areas of your heart are chronically deprived of oxygen and nutrients because of reduced blood flow, or if your heart has been damaged by a heart attack, your heart may become too weak to pump enough blood to meet your body's needs. This condition is known as heart failure.
- Abnormal heart rhythm (arrhythmia). Inadequate blood supply to the heart or damage to heart tissue can interfere with your heart's electrical impulses, causing abnormal heart rhythms
Tests and diagnosis
Electrocardiogram (ECG).An electrocardiogram records electrical signals as they travel through your heart. An ECG can often reveal evidence of a previous heart attack or one that's in progress.The doctor will ask questions about your medical history, do a physical exam and order routine blood tests. He or she may suggest one or more diagnostic tests as well, including:
- In other cases, Holter monitoring may be recommended. With this type of ECG, you wear a portable monitor for 24 hours as you go about your normal activities. Certain abnormalities may indicate inadequate blood flow to your heart.
- Echocardiogram. An echocardiogram uses sound waves to produce images of your heart. During an echocardiogram, your doctor can determine whether all parts of the heart wall are contributing normally to your heart's pumping activity. Parts that move weakly may have been damaged during a heart attack or be receiving too little oxygen. This may indicate coronary artery disease or various other conditions.
- Stress test. If your signs and symptoms occur most often during exercise, your doctor may ask you to walk on a treadmill or ride a stationary bike during an ECG. This is known as an exercise stress test. In some cases, medication to stimulate your heart may be used instead of exercise.Some stress tests are done using an echocardiogram. For example, your doctor may do an ultrasound before and after you exercise on a treadmill or bike. Or your doctor may use medication to stimulate your heart during an echocardiogram.Another stress test known as a nuclear stress test helps measure blood flow to your heart muscle at rest and during stress. It's similar to a routine exercise stress test but with images in addition to an ECG. Trace amounts of radioactive material such as thallium are injected into your bloodstream. Special cameras can detect areas in your heart that receive less blood flow.
- Cardiac catheterization or angiogram. To view blood flow through your heart, your doctor may inject a special dye into your arteries (intravenously). This is known as an angiogram. The dye is injected into the arteries of the heart through a long, thin, flexible tube (catheter) that is threaded through an artery, usually in the leg, to the arteries in the heart.This procedure is called cardiac catheterization. The dye outlines narrow spots and blockages on the X-ray images. If you have a blockage that requires treatment, a balloon can be pushed through the catheter and inflated to improve the blood flow in your coronary arteries. A mesh tube (stent) may then be used to keep the dilated artery open.
- Heart scan. Computerized tomography (CT) technologies can help your doctor see calcium deposits in your arteries that can narrow the arteries. If a substantial amount of calcium is discovered, coronary artery disease may be likely.A CT coronary angiogram, in which you receive a contrast dye injected intravenously during a CT scan, also can generate images of your heart arteries.
- Magnetic resonance angiography (MRA). This procedure uses MRI technology, often combined with an injected contrast dye, to check for areas of narrowing or blockages — although the details may not be as clear as those provided by coronary catheterization.
Lifestyle and home remedies
Lifestyle changes can help you prevent or slow the progression of coronary artery disease.
- Stop smoking. Smoking is a major risk factor for coronary artery disease. Nicotine constricts blood vessels and forces your heart to work harder, and carbon monoxide reduces oxygen in your blood and damages the lining of your blood vessels. If you smoke, quitting is one of the best ways to reduce your risk of a heart attack.
- Control your blood pressure. Ask your doctor for a blood pressure measurement at least every two years. He or she may recommend more frequent measurements if your blood pressure is higher than normal or you have a history of heart disease. The ideal blood pressure is below 120 systolic and 80 diastolic, as measured in millimeters of mercury (mm Hg).
- Check your cholesterol. Ask your doctor for a baseline cholesterol test when you're in your 20s and at least every five years after. If your test results aren't within desirable ranges, your doctor may recommend more-frequent measurements. Most people should aim for an LDL level below 130 milligrams per deciliter (mg/dL), or 3.4 millimoles per liter (mmol/L). If you have other risk factors for heart disease, your target LDL may be below 100 mg/dL (2.6 mmol/L).
- Keep diabetes under control. If you have diabetes, tight blood sugar control can help reduce the risk of heart disease.
- Get moving. Exercise helps you achieve and maintain a healthy weight and control diabetes, elevated cholesterol and high blood pressure — all risk factors for coronary artery disease. With your doctor's OK, aim for 30 to 60 minutes of physical activity most or all days of the week.
- Eat healthy foods. A heart-healthy diet, such as the Mediterranean diet, that emphasizes plant-based foods, such as fruits, vegetables, whole grains, legumes and nuts — and is low in saturated fat, cholesterol and sodium — can help you control your weight, blood pressure and cholesterol. Eating one or two servings of fish a week also is beneficial.
- Maintain a healthy weight. Being overweight increases your risk of coronary artery disease. Losing even just a few pounds can help lower your blood pressure and reduce your risk of coronary artery disease.
- Manage stress. Reduce stress as much as possible. Practice healthy techniques for managing stress, such as muscle relaxation and deep breathing.
In addition to healthy lifestyle changes, remember the importance of regular medical checkups. Some of the main risk factors for coronary artery disease — high cholesterol, high blood pressure and diabetes — have no symptoms in the early stages. Early detection and treatment can set the stage for a lifetime of better heart health.
Also ask your doctor about a yearly flu vaccine. Coronary artery disease and other cardiovascular disorders increase the risk of complications from the flu.
Prevention
The same lifestyle habits that can help treat coronary artery disease can also help prevent it from developing in the first place. Leading a healthy lifestyle can help keep your arteries strong and clear of plaques. To improve your heart health, you can:
- Quit smoking
- Control conditions such as high blood pressure, high cholesterol and diabetes
- Stay physically active
- Eat a low-fat, low-salt diet that's rich in fruits, vegetables and whole grains
- Maintain a healthy weight
- Reduce and manage stress






.jpg)



.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)




No comments:
Post a Comment