Glaucoma
Glaucoma is a term describing a group of ocular disorders with multi-factorial etiology united by a clinically characteristic intraocular pressure-associated optic neuropathy.[1] This can permanently damage vision in the affected eye(s) and lead to blindness if left untreated. It is normally associated with increased fluid pressure in the eye (aqueous humour).[2] The term "ocular hypertension" is used for people with consistently raised intraocular pressure (IOP) without any associated optic nerve damage. Conversely, the term 'normal tension' or 'low tension' glaucoma is used for those with optic nerve damage and associated visual field loss, but normal or low IOP.
The nerve damage involves loss of retinal ganglion cells in a characteristic pattern. The many different subtypes of glaucoma can all be considered to be a type of optic neuropathy. Raised intraocular pressure (above 21 mmHg or 2.8 kPa) is the most important and only modifiable risk factor for glaucoma. However, some may have high eye pressure for years and never develop damage, while others can develop nerve damage at a relatively low pressure. Untreated glaucoma can lead to permanent damage of the optic nerveand resultant visual field loss, which over time can progress to blindness.
Glaucoma can be roughly divided into two main categories, "open-angle" and "closed-angle" (or "angle closure") glaucoma. The angle refers to the area between the iris and cornea, through which fluid must flow to escape via the trabecular meshwork. Closed-angle glaucoma can appear suddenly and is often painful; visual loss can progress quickly, but the discomfort often leads patients to seek medical attention before permanent damage occurs. Open-angle, chronic glaucoma tends to progress at a slower rate and patients may not notice they have lost vision until the disease has progressed significantly.
When the scleral venous sinus is blocked to where aqueous humor is not reabsorbed at a faster rate than it is being secreted, elevated pressure within the eye occurs. Pressure in the anterior and posterior chambers pushes the lens back and puts pressure on the vitreous body. The vitreous body presses the retina against the choroid and compresses the blood vessels that feed the retina. Without a sufficient blood supply, retinal cells will die and the optic nerve may atrophy, causing blindness.[3] Typically, the nerves furthest from the focal point fail first because of their distance from the central blood supply to the eye; thus, vision loss due to glaucoma tends to start at the edges with the peripheral visual field, leading to progressively worse tunnel vision.[4]
Glaucoma has been called the "silent thief of sight" because the loss of vision often occurs gradually over a long period of time, and symptoms only occur when the disease is quite advanced. Once lost, vision cannot normally be recovered, so treatment is aimed at preventing further loss. Worldwide, glaucoma is the second-leading cause of blindness after cataracts.[5][6] It is also the leading cause of blindness among African Americans.[7] Glaucoma affects one in 200 people aged 50 and younger, and one in 10 over the age of eighty. If the condition is detected early enough, it is possible to arrest the development or slow the progression with medical and surgical means.
The word "glaucoma" comes from the Greek γλαύκωμα, "opacity of the crystalline lens". (Cataracts and glaucoma were not distinguished until c. 1705.[8])
Signs and symptoms
The two main types of glaucoma are open-angle glaucoma and closed-angle glaucoma (also called angle closure glaucoma). Open-angle glaucoma accounts for 90% of glaucoma cases in the United States. It is painless and does not have acute attacks. The only signs are gradually progressive visual field loss, and optic nerve changes (increased cup-to-disc ratio on fundoscopic examination).
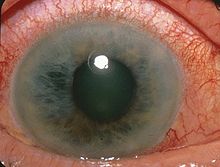
Closed-angle glaucoma accounts for less than 10% of glaucoma cases in the United States, but as many as half of glaucoma cases in other nations (particularly Asian countries). About 10% of patients with closed angles present with acute angle closure crises characterized by sudden ocular pain, seeing halos around lights, red eye, very high intraocular pressure (>30 mmHg), nausea and vomiting, suddenly decreased vision, and a fixed, mid-dilated pupil. It is also associated with an oval pupil in some cases. Acute angle closure is an emergency.
Causes
Of the several causes for glaucoma, ocular hypertension (increased pressure within the eye) is the most important risk factor in most glaucomas, but in some populations, only 50% of people with primary open-angle glaucoma actually have elevated ocular pressure.[9]
Dietary
No clear evidence indicates vitamin deficiencies cause glaucoma in humans. It follows, then, that oral vitamin supplementation is not a recommended treatment for glaucoma.[10] Caffeine increases intraocular pressure in those with glaucoma, but does not appear to affect normal individuals.[11]
Ethnicity and sex
Many people of East Asian descent are prone to developing angle closure glaucoma due to shallower anterior chamber depths, with the majority of cases of glaucoma in this population consisting of some form of angle closure.[12] Inuit also have a 20 to 40 times higher risk of developing primary angle closure glaucoma. Women are three times more likely than men to develop acute angle closure glaucoma due to their shallower anterior chambers. People of African descent are three times more likely to develop primary open angle glaucoma.
Genetics
Positive family history is a risk factor for glaucoma. The relative risk of having primary open angle glaucoma (POAG) is increased approximately 2–4 fold for individuals who have a sibling with glaucoma.[13] Glaucoma, particularly primary open angle glaucoma, is associated with mutations in several different genes (including MYOC, ASB10, WDR36, NTF4, TBK1 genes),[14] although most cases of glaucoma do not involve these genetic mutations. Normal tension glaucoma, which comprises one-third of POAG, is also associated with genetic mutations (including OPA1 and OPTN genes).[15]
Various rare congenital/genetic eye malformations are associated with glaucoma. Occasionally, failure of the normal third trimester gestational atrophy of the hyaloid canal and the tunica vasculosa lentis is associated with other anomalies. Angle closure-induced ocular hypertension and glaucomatous optic neuropathy may also occur with these anomalies,[16][17][18] and has been modelled in mice.[19]
Other
Other factors can cause glaucoma, known as "secondary glaucomas", including prolonged use of steroids (steroid-induced glaucoma); conditions that severely restrict blood flow to the eye, such as severe diabetic retinopathy and central retinal vein occlusion (neovascular glaucoma); ocular trauma (angle recession glaucoma); and uveitis (uveitic glaucoma). In a large study in the UK, glaucoma patients had a 29% increased incidence of systemic hypertension compared to age- and sex-matched controls.[20]
Pathophysiology
The underlying cause of open-angle glaucoma remains unclear. Several theories exist on its exact etiology. However, the major risk factor for most glaucomas, and the focus of treatment, is increased intraocular pressure, i.e. ocular hypertension. Intraocular pressure is a function of production of liquid aqueous humor by the ciliary processes of the eye, and its drainage through the trabecular meshwork. Aqueous humor flows from the ciliary processes into the posterior chamber, bounded posteriorly by the lens and the zonules of Zinn, and anteriorly by the iris. It then flows through the pupil of the iris into the anterior chamber, bounded posteriorly by the iris and anteriorly by the cornea. From here, the trabecular meshwork drains aqueous humor via Schlemm's canal into scleral plexuses and general blood circulation.[21]
In open/wide-angle glaucoma, flow is reduced through the trabecular meshwork, due to the degeneration and obstruction of the trabecular meshwork, whose original function is to absorb the aqueous humor. Loss of aqueous humor absorption leads to increased resistance and thus a chronic, painless buildup of pressure in the eye.[22] In close/narrow-angle, the iridocorneal angle is completely closed because of forward displacement of the final roll and root of the iris against the cornea, resulting in the inability of the aqueous fluid to flow from the posterior to the anterior chamber and then out of the trabecular network. This accumulation of aqueous humor causes an acute increase of pressure and pain.
The inconsistent relationship of glaucomatous optic neuropathy with ocular hypertension has provoked hypotheses and studies on anatomic structure, eye development, nerve compression trauma, optic nerve blood flow, excitatory neurotransmitter, trophic factor, retinal ganglion cell/axon degeneration, glial support cell, immune system, aging mechanisms of neuron loss, and severing of the nerve fibers at the scleral edge.
Diagnosis
Screening for glaucoma is usually performed as part of a standard eye examination performed by optometrists, orthoptists and ophthalmologists. Testing for glaucoma should include measurements of the intraocular pressure via tonometry, changes in size or shape of the eye, anterior chamber angle examination or gonioscopy, and examination of the optic nerve to look for any visible damage to it, or change in the cup-to-disc ratio and also rim appearance and vascular change. A formal visual field test should be performed. The retinal nerve fiber layer can be assessed with imaging techniques such as optical coherence tomography, scanning laser polarimetry, and/or scanning laser ophthalmoscopy.[35][36]
Owing to the sensitivity of all methods of tonometry to corneal thickness, methods such as Goldmann tonometry should be augmented with pachymetry to measure central corneal thickness (CCT). A thicker-than-average cornea can result in a pressure reading higher than the 'true' pressure, whereas a thinner-than-average cornea can produce a pressure reading lower than the 'true' pressure.
Because pressure measurement error can be caused by more than just CCT (i.e., corneal hydration, elastic properties, etc.), it is impossible to 'adjust' pressure measurements based only on CCT measurements. The frequency doubling illusion can also be used to detect glaucoma with the use of a frequency doubling technology perimeter.[37]
Examination for glaucoma also could be assessed with more attention given to sex, race, history of drug use, refraction, inheritance and family history.[35]
| What Test Examines | How Examination is Accomplished | |
|---|---|---|
| Tonometry | Inner eye pressure | The eye is numbed via eye drops. The examiner then uses a tonometer to measure the inner pressure of the eye through pressure applied by a puff of warm air or a tiny tool. |
| Ophthalmoscopy(dilated eye exam) | Shape and color of the optic nerve | The pupil is dilated via the application of eye drops. Using a small magnification device with a light on the end, the examiner can examine the magnified optic nerve. |
| Perimetry (visual field test) | Complete field of vision | The patient looks straight ahead and is asked to indicate when light passes the patient's peripheral field of vision. This allows the examiner to map the patient’s field of vision. |
| Gonioscopy | Angle in the eye where the iris meets the cornea | Eye drops are used to numb the eye. A hand-held contact lens with a mirror is placed gently on the eye to allow the examiner to see the angle between the cornea and the iris. |
| Pachymetry | Thickness of the cornea | The examiner places a pachymeter gently on the front of the eye to measure its thickness. |
| Nerve fiber analysis | Thickness of the nerve fiber layer | Using one of several techniques, the nerve fibers are examined. |
Screening
The United States Preventive Services Task Force as of 2013 states there is insufficient evidence to recommend for or against screening for glaucoma.[41] There is thus no national screening programs in the US. There is in the UK. Those at risk are advised to have a dilated eye examination at least once a year.[42]
Management
The modern goals of glaucoma management are to avoid glaucomatous damage and nerve damage, and preserve visual field and total quality of life for patients, with minimal side effects.[43][44] This requires appropriate diagnostic techniques and follow-up examinations, and judicious selection of treatments for the individual patient. Although intraocular pressure is only one of the major risk factors for glaucoma, lowering it via various pharmaceuticals and/or surgical techniques is currently the mainstay of glaucoma treatment.
Vascular flow and neurodegenerative theories of glaucomatous optic neuropathy have prompted studies on various neuroprotective therapeutic strategies, including nutritional compounds, some of which may be regarded by clinicians as safe for use now, while others are on trial.
Balance and postural control
in balance and maintaining posture in human beings, glaucoma patients should consider themselves at greater risk of falls, and would be advised to take the necessary precautions to help prevent any accidents. In addition, since the peripheral visual system has such a high contribution to this intrinsic balancing mechanism, the severity of glaucoma and degree of visual field obstruction should also be considered.[45] Because of the relationship of glaucoma with age, other associated factors affecting balance (i.e. impaired proprioception) may also be present, further increasing the risk of falls. Of interesting note, one cohort of open-angle glaucoma patients had their ability to maintain posture measured (via measurements of sway) in binocular (two-eyed) and monocular (one-eyed, using both affected and unaffected eyes) conditions, as well as with their eyes closed. These patients had increased sway (worse balance) in their one-eyed conditions compared to the two-eyed conditions, and reduced sway (better balance) when using one eye than when their eyes were closed, but there were no significant differences between the two monocular conditions, with the unaffected eye having only slightly (but not significantly) reduced sway than when using their affected eyes. All patients in each condition displayed increased sway compared to their age-matched controls.[46]
Medication
Intraocular pressure can be lowered with medication, usually eye drops. Several different classes of medications are used to treat glaucoma, with several different medications in each class.
Each of these medicines may have local and systemic side effects. Adherence to medication protocol can be confusing and expensive; if side effects occur, the patient must be willing either to tolerate them, or to communicate with the treating physician to improve the drug regimen. Initially, glaucoma drops may reasonably be started in either one or in both eyes.[47]
Poor compliance with medications and follow-up visits is a major reason for vision loss in glaucoma patients. A 2003 study of patients in an HMO found half failed to fill their prescriptions the first time, and one-fourth failed to refill their prescriptions a second time.[48] Patient education and communication must be ongoing to sustain successful treatment plans for this lifelong disease with no early symptoms.
The possible neuroprotective effects of various topical and systemic medications are also being investigated.[10][49][50][51]
- Prostaglandin analogs, such as latanoprost (Xalatan), bimatoprost (Lumigan) and travoprost (Travatan), increase uveoscleral outflow of aqueous humor. Bimatoprost also increases trabecular outflow.
- Topical beta-adrenergic receptor antagonists, such as timolol, levobunolol (Betagan), and betaxolol, decrease aqueous humor production by the ciliary body.
- Alpha2-adrenergic agonists, such as brimonidine (Alphagan) and apraclonidine, work by a dual mechanism, decreasing aqueous humor production and increasing uveoscleral outflow.
- Less-selective alpha agonists, such as epinephrine, decrease aqueous humor production through vasoconstriction of ciliary body blood vessels, useful only in open-angle glaucoma. Epinephrine's mydriatic effect, however, renders it unsuitable for closed-angle glaucoma due to further narrowing of the uveoscleral outflow (i.e. further closure of trabecular meshwork, which is responsible for absorption of aqueous humor).
- Miotic agents (parasympathomimetics), such as pilocarpine, work by contraction of the ciliary muscle, opening the trabecular meshwork and allowing increased outflow of the aqueous humour. Echothiophate, an acetylcholinesterase inhibitor, is used in chronic glaucoma.
- Carbonic anhydrase inhibitors, such as dorzolamide (Trusopt), brinzolamide (Azopt), and acetazolamide (Diamox), lower secretion of aqueous humor by inhibiting carbonic anhydrase in the ciliary body.
- Physostigmine is also used to treat glaucoma.
- Marijuana was found, in the early 1970s, to reduce pressure in the eyes, though how the cannabinoids in marijuana produce this effect remains unknown.
Surgery
Main article: Glaucoma surgery
Both laser and conventional surgeries are performed to treat glaucoma. Surgery is the primary therapy for those with congenitalglaucoma.[52] Generally, these operations are a temporary solution, as there is not yet a cure for glaucoma.
Canaloplasty
Canaloplasty is a nonpenetrating procedure using microcatheter technology. To perform a canaloplasty, an incision is made into the eye to gain access to the Schlemm's canal in a similar fashion to a viscocanalostomy. A microcatheter will circumnavigate the canal around the iris, enlarging the main drainage channel and its smaller collector channels through the injection of a sterile, gel-like material called viscoelastic. The catheter is then removed and a suture is placed within the canal and tightened.
By opening the canal, the pressure inside the eye may be relieved, although the reason is unclear, since the canal (of Schlemm) does not have any significant fluid resistance in glaucoma or healthy eyes. Long-term results are not available.[53][54]
Laser surgery
Argon laser trabeculoplasty (ALT) may be used to treat open-angle glaucoma. It is a temporary solution, not a cure. A 50-μm argon laser spot is aimed at the trabecular meshwork to stimulate opening of the mesh to allow more outflow of aqueous fluid. Usually, half of the angle is treated at a time. Traditional laser trabeculoplasty uses a thermal argon laser in an argon laser trabeculoplasty procedure.
A newer type of laser trabeculoplasty uses a "cold" (nonthermal) laser to stimulate drainage in the trabecular meshwork. This newer procedure, selective laser trabeculoplasty (SLT), uses a 532-nm, frequency-doubled, Q-switched Nd:YAG laser, which selectively targets melanin pigment in the trabecular meshwork cells. Studies show SLT is as effective as ALT at lowering eye pressure. In addition, SLT may be repeated three to four times, whereas ALT can usually be repeated only once.
Nd:YAG laser peripheral iridotomy (LPI) may be used in patients susceptible to or affected by angle closure glaucoma or pigment dispersion syndrome. During laser iridotomy, laser energy is used to make a small, full-thickness opening in the iris to equalize the pressure between the front and back of the iris, thus correcting any abnormal bulging of the iris. In people with narrow angles, this can uncover the trabecular meshwork. In some cases of intermittent or short-term angle closure, this may lower the eye pressure. Laser iridotomy reduces the risk of developing an attack of acute angle closure. In most cases, it also reduces the risk of developing chronic angle closure or of adhesions of the iris to the trabecular meshwork.
Diode laser cycloablation lowers IOP by reducing aqueous secretion by destroying secretory ciliary epithelium.[35]
Trabeculectomy
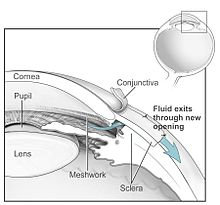
The most common conventional surgery performed for glaucoma is the trabeculectomy. Here, a partial thickness flap is made in the scleral wall of the eye, and a window opening is made under the flap to remove a portion of the trabecular meshwork. The scleral flap is then sutured loosely back in place to allow fluid to flow out of the eye through this opening, resulting in lowered intraocular pressure and the formation of a bleb or fluid bubble on the surface of the eye. Scarring can occur around or over the flap opening, causing it to become less effective or lose effectiveness altogether. Traditionally, chemotherapeutic adjuvants, such as mitomycin C (MMC, 0.5–0.2 mg/ml) or 5-fluorouracil (5-FU, 50 mg/ml), are applied with soaked sponges on the wound bed to prevent filtering blebs from scarring by inhibiting fibroblast proliferation. Contemporary alternatives include the sole or combinative implementation of nonchemotherapeutic adjuvants, such as collagen matrix implant[55][56][57][58] or other biodegradable spacers, to prevent super scarring by randomization and modulation of fibroblast proliferation in addition to the mechanical prevention of wound contraction and adhesion.
Glaucoma drainage implants
Main article: Glaucoma valve
Professor Anthony Molteno developed the first glaucoma drainage implant, in Cape Town in 1966.[59] Since then, several different types of implants have followed on from the original, the Baerveldt tube shunt, or the valved implants, such as the Ahmed glaucoma valve implant or the ExPress Mini Shunt and the later generation pressure ridge Molteno implants. These are indicated for glaucoma patients not responding to maximal medical therapy, with previous failed guarded filtering surgery (trabeculectomy). The flow tube is inserted into the anterior chamber of the eye, and the plate is implanted underneath the conjunctiva to allow flow of aqueous fluid out of the eye into a chamber called a bleb.
- The first-generation Molteno and other nonvalved implants sometimes require the ligation of the tube until the bleb formed is mildly fibrosed and water-tight.[60] This is done to reduce postoperative hypotony—sudden drops in postoperative intraocular pressure.
- Valved implants, such as the Ahmed glaucoma valve, attempt to control postoperative hypotony by using a mechanical valve.
The ongoing scarring over the conjunctival dissipation segment of the shunt may become too thick for the aqueous humor to filter through. This may require preventive measures using antifibrotic medications, such as 5-fluorouracil or mitomycin-C (during the procedure), or other nonantifibrotic medication methods, such as collagen matrix implant,[61][62] or biodegradable spacer, or later on create a necessity for revision surgery with the sole or combinative use of donor patch grafts or collagen matrix implant.[63][64] And for glaucomatous painful blind eye and some cases of glaucoma, cyclocryotherapy for ciliary body ablation could be considered to be performed.[65]
Veterinary implant
TR BioSurgical has commercialized a new implant specifically for veterinary medicine, called TR-ClarifEYE. The implant consists of a new biomaterial, the STAR BioMaterial, which consists of silicone with a very precise homogenous pore size, a property which reduces fibrosis and improves tissue integration. The implant contains no valves and is placed completely within the eye without sutures. To date, it has demonstrated long-term success (longer than a year) in a pilot study in medically refractory dogs with advanced glaucoma.[66]
Laser-assisted nonpenetrating deep sclerectomy
The most common surgical approach currently used for the treatment of glaucoma is trabeculectomy, in which the sclera is punctured to alleviate intraocular pressure.
Nonpenetrating deep sclerectomy (NPDS) surgery is a similar, but modified, procedure, in which instead of puncturing the scleral bed and trabecular meshwork under a scleral flap, a second deep scleral flap is created, excised, with further procedures of deroofing the Schlemm's canal, upon which, percolation of liquid from the inner eye is achieved and thus alleviating intraocular pressure, without penetrating the eye. NPDS is demonstrated to cause significantly fewer side effects than trabeculectomy.[citation needed] However, NPDS is performed manually and requires higher level of skills that may be assisted with instruments.[citation needed] In order to prevent wound adhesion after deep scleral excision and to maintain good filtering results, NPDS as with other non-penetrating procedures is sometimes performed with a variety of biocompatible spacer or devices, such as the Aquaflow collagen wick,[67] ologen Collagen Matrix,[68][69][70] or Xenoplast glaucoma implant.[71]
Laser-assisted NPDS is performed with the use of a CO2 laser system. The laser-based system is self-terminating once the required scleral thickness and adequate drainage of the intraocular fluid have been achieved. This self-regulation effect is achieved as the CO2 laser essentially stops ablating as soon as it comes in contact with the intraocular percolated liquid, which occurs as soon as the laser reaches the optimal residual intact layer thickness.
Epidemiology
As of 2010, there were 44.7 million people in the world with open angle glaucoma.[73] The same year, there were 2.8 million people in the United States with open angle glaucoma.[73] By 2020, the prevalence is projected to increase to 58.6 million worldwide and 3.4 million the United States.[73]
Internationally, glaucoma is the second-leading cause of blindness, after cataracts. Glaucoma is also the leading cause of blindness in African Americans, who have higher rates of primary open angle glaucoma.[74] Bilateral vision loss can negatively affect mobility and interfere with driving.[75]
A meta-analysis published in 2009 found that patients with primary open angle glaucoma do not have increased mortality rates, or increased risk of cardiovascular death.







.jpg)







.jpg)
.jpg)
.jpg)
.jpg)




No comments:
Post a Comment